Low-density lipoprotein (LDL) cholesterol accumulation is the leading problem for various cardiovascular diseases. Besides high cholesterol levels, high sugar levels, and high blood pressure also affect the heart critically. But what leads to Congestive Heart Failure (CHF)? In the context of heart problems, most of them are the leading causes of one another. For instance, Coronary Artery disease (CAD) leads to myocardial infarction which in turn makes heart muscles weak and dilated. The weakening of heart muscles provokes the situation for congestive heart failure. We will learn the salient disparities among thrice of them later. First, we will apprehend the context of congestive heart failure and what leads to congestive heart failure.
Table of contents
General Understanding of the Heart’s Structure
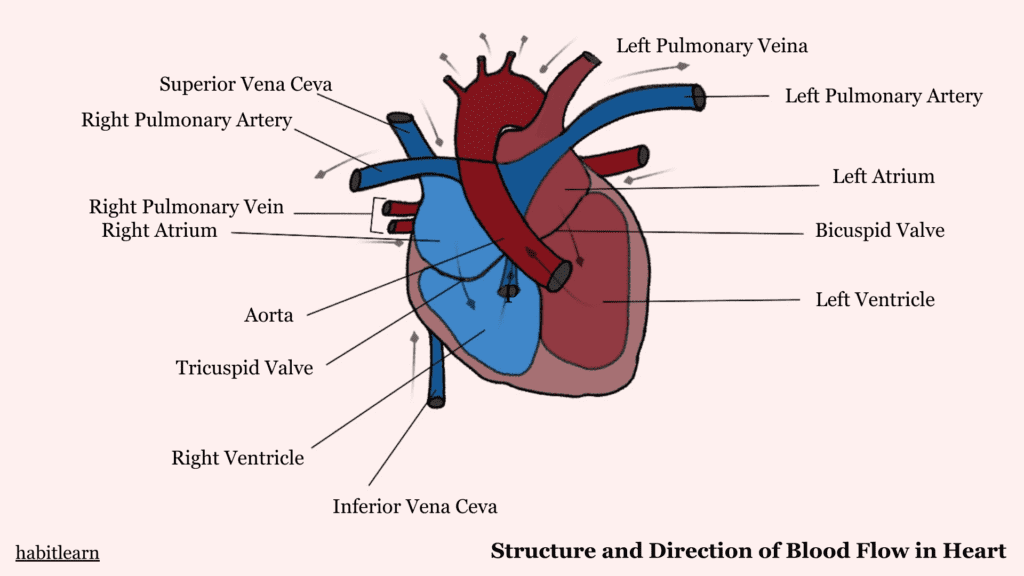
The heart is a muscular organ due to the integral participation of the myocardium ( Middle layer of the heart). Specialized muscles- the cardiac muscles make the myocardium of the heart. The resilient and elastic nature of the myocardium makes the heart a potent muscular organ. The heart is divided into four chambers; two upper atria and two lower ventricles. Deoxygenated blood from the body pours into the right atrium while the oxygenated blood from the lungs pours into the left atrium.
Interatrial valves ensure the separation of blood. The right ventricle pumps blood into the lungs for oxygenation through pulmonary arteries and the left ventricle pumps the blood to the whole body. Now, let’s delve into the understanding of congestive heart failure and what leads to congestive heart failure.
Types of Heart Failures
Before getting drenched into congestive heart failure, one must know the types of heart failure.
1. Systolic Heart Failure
As its name suggests, systolic heart failure results from the impaired contrative activity of the heart’s left ventricle. In this type of heart failure, the muscular walls of the left ventricle become weak, and the heart becomes impotent to pump blood effectively through it. Consequently, cardiac output is reduced and leads to insufficient blood supply to the body.
2. Diastolic Heart Failure
Diastolic heart failure occurs when the heart is unable to relax properly. Compromised relaxation of the heart causes variations in normal heart rhythms instigates arrhythmias. The left ventricle becomes stiff and rigid due to increased blood pressure. This feature of the left ventricle makes it difficult to relax appropriately in regular contractions. Due to the less filing time, the left ventricle pumps reduced blood volume to the systemic circulation.
What is congestive heart failure?
Congestive heart failure is the inefficient pumping ability of the heart. Heart muscles become weakened, damaged, or can die with the severity of failure. Lack of oxygen and nutrient supply to the heart muscles triggers the impairment or death of the respective heart muscles. When one or more parts of the heart become non-functional, it affects the overall pumping ability of the heart. Due to insufficient pumping action of the heart, cardiac output is reduced and multiple organs have to suffer from insufficient blood supply.
Kidneys, lungs, and the heart itself are most affected by congestive heart failure. Due to low blood volume in arteries, kidneys retain fluid by reabsorbing sodium and water from the tubules. This reabsorption leads to fluid retention in blood vessels which is a problematic aftermath of heart failure.
What leads to congestive heart failure?
The following are the most obvious causes of congestive heart failure;
Atherosclerosis
High cholesterol content in the body leads to the deposition of lipids in the blood vessels. Deposition of fatty acids, calcium, and some other substances provokes the formation of plaques in the inner lining of blood vessels. This scenario makes the blood vessels narrow and stiff leading to atherosclerosis. Read which foods contain low -density lipoprotein (LDL) cholesterol that lead to the formation of fatty deposits. The formation of plaques perturbs the normal flow of blood and severe conditions lead to blockage of the respective blood vessels.
Atherosclerosis disrupts the normal functionality of an organ or the body part to which this blocked vessel is supplying blood. Lack of oxygen and nutrient supply due to impaired blood flow creates alarm for the respective body part. In the heart failure case, the formation of cholesterol deposits in the arteries supplying blood to the heart muscles upsets their nutritional demand. As a result, the respective heart muscle can die, affecting the heart’s normal functionality.
Coronary Artery Disease
The formation of atherosclerotic plaques in the coronary arteries (arteries that supply oxygenated blood to the heart ) gives rise to coronary artery disease. Plaques offer resistance to normal blood flow and impair the delivery of oxygen and other nutrients to the desired location. Sometimes, these plaques get unstable and rupture inside the arteries. Rupturing of plaques provokes the formation of blood clots (thrombosis) when blood cells get attached to the plaque’s surface. Large blood clots block the coronary arteries completely and terminate the blood supply to the respective heart muscle. As a result of this, the heart muscle dies (Myocardial infarction) due to lack of oxygen for a prolonged period.
Myocardial infarction is the impairment or ultimate death of the heart muscle due to blockage in the coronary artery supplying blood to that muscle. Damage or death of a heart’s muscle affects the overall pumping ability of the heart. When a heart muscle is damaged, it releases specific enzymes into the bloodstream; troponin and creatine kinase. High levels of these enzymes can cause the upsetting of heart muscle. As long as this destruction persists, the heart becomes weak and prompts failure if not treated adequately.
Hypertension
Hypertension or high blood pressure is a grave condition in itself. It does not only give rise to congestive heart failure but can also induce complications for the kidneys and lungs. High blood pressure makes the heart function over-efficient due to increased resistance. Blood pressure is the pressure exerted by the blood volume to the arterial walls. Increased blood pressure elevates the workload of the heart. The left ventricle has to pump blood more forcefully than normal. Consequently, muscles of the left ventricle become enlarged and dilated, affecting the integrity of muscles. Left ventricular hypertrophy (LVH) is the most common condition that arises from high blood pressure.
LVH is characterized by enlargement and weakening of the left ventricle due to high workload as an adaptive strategy. This adaptive strategy seems good at first as it makes the heart able to pump excess blood volume but later this strategy causes the weakening of the left ventricle, affecting its pumping action. The left ventricle becomes rigid and does not relax properly during contractions. Impaired relaxations trigger irregular heart beats- arrhythmias.
Cardiomyopathy
Cardiomyopathy is the weakening or stiffening of heart muscles. Various factors like genetics, alcohol consumption, and nutritional deficiencies directly impact the health of cardiac muscles. Besides these obvious causes, high blood pressure or myocardial infarction also leads to impairment of heart muscles. The most common target of cardiomyopathy are left ventricular muscles as they have the utmost function of supplying blood to the entire body. Left ventricular hypertrophy (LVH) makes the left ventricle meager to pump blood efficiently.
Coronary artery disease hinders the rush of blood to the cardiac muscles. Affected cardiac muscle deteriorates with time due to lacking oxygen and other nutrients. Impaired cardiac muscle affects the overall cardiac contractility. As an answer to the question of what leads to congestive heart failure, cardiomyopathy is the main contributor to congestive heart failure.
Chronic Obstructive Pulmonary Disease
I can write a complete 2500-word blog on this topic, but here in order to keep it short, COPD is defined as impaired lung functioning. Due to fluid buildup in the lungs, its gas-exchanging effectivity is compromised. It builds up pressure in pulmonary arteries that carry deoxygenated blood from the heart’s right ventricle to the lungs for oxygenation. Pulmonary hypertension (elevated blood pressure in the pulmonary arteries due to congestion in the lungs.) disturbs the right ventricle’s functionality. High blood pressure in pulmonary arteries prompts the backflow of blood into systemic circulation. This backflow leads to fluid retention in the weight-bearing parts of the body.
As a result of fluid retention, blood vessels become congested due to increased blood volume in them. Elevated blood pressure puts strain on the left ventricle and provokes congestive heart failure. Reduced cardiac output in congestive heart failure further aggravates the pulmonary impairment. COPD and CHF interplay with each other and lead to the declining spiral of health.
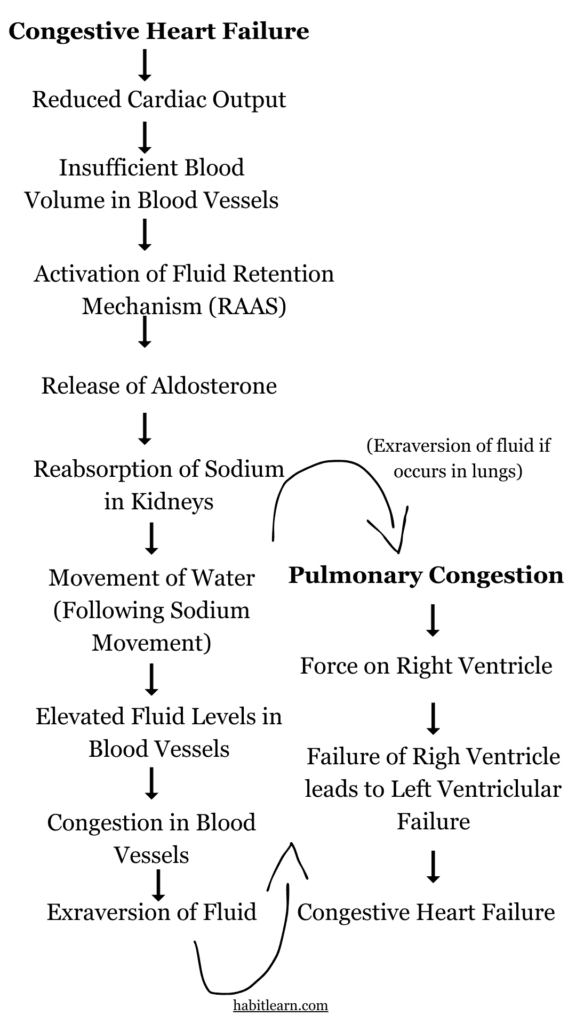
The Major Consequence of Congestive Heart Failure – Fluid Retention
Fluid retention exacerbates congestive heart failure as both of them are interconnected. Reduced cardiac output due to left ventricular hypertrophy is incompetent to meet the body’s demand for blood supply. Due to less blood volume in blood vessels, our body stimulates the fluid retention mechanisms(RAAS). For this purpose, adrenal glands secrete aldosterone which reabsorb sodium from the kidney tubules. Water, in turn follows the concentration gradient and retains the fluid in blood vessels. Fluid retention becomes critical for health when this fluid leaks into the interstitial spaces of cells due to increased pressure.
Elevated fluid pressure inside blood vessels induces congestion and obfuscates the the lung’s exchanging mechanism. Congestion in the lungs (pulmonary congestion) is much more severe as it affects our breathing and also disturbs the optimal functioning of the right ventricle. The detailed relationship between pulmonary congestion and right ventricular failure is discussed under the Chronic Obstructive Pulmonary Disease section.



You revealed this well.